This patient was an 82-year-old
former smoker who was living in a
care home. He had an ulcer on the
side of his left foot that had been
present for one week and measured
2x1cm with 100% granulating tissue
in the wound bed (
Figure 1
).
The patient tested negative
for diabetes after a blood test and
his ankle brachial pressure index
(ABPI) was also measured and
found to be normal, with a clear
signal indicating a lack of arterial
involvement.
Overall, there was no underlying
medical condition that might have
delayed healing. The periwound skin
was also healthy and he was not
experiencing any pain.
Wound progression
Actilite Protect (10x10cm) was
used to cover the wound, and,
although the clinician reported that
CASE REPORT 5
This case details how a honey-
based dressing was used as
an all-in-one treatment option
in the case of patient with a
foot ulcer.
this size initially seemed too large,
the dressing did conform well to
the wound. While the dimensions
of the wound did not change
dramatically over the two-week
evaluation period, it did show signs
of improvement (
Figures 2
and
3
).
Dressings were changed every
four days throughout the evaluation
and were reported to be easy to
use and to remove, being rated
‘3’ on a five-point scale for ease
of application, with ‘1’ indicating
very easy removal and ‘5’ very
difficult removal. The dressing was
atraumatic to the wound bed and
the periwound skin and the patient
did not experience any pain during
application or removal.
Over the evaluation period,
the dressing remained intact on
removal and stayed in place as long
as expected, with no rolling at the
edges. The clinician felt that the
dressing had positively contributed
to wound healing and that it was
easy to use because of its all-in-one
composition (foam, Manuka honey
and a silicone wound contact layer).
However, the clinician did
comment about the sizes available,
saying that smaller-sized dressings
would be a useful option.
The patient found the dressing
very comfortable to wear and was
very satisfied with the pain-free
treatment he had received during
the two-week evaluation.
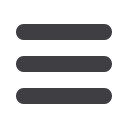
Figure 2.
The wound showing an increase
in epithelialisation.
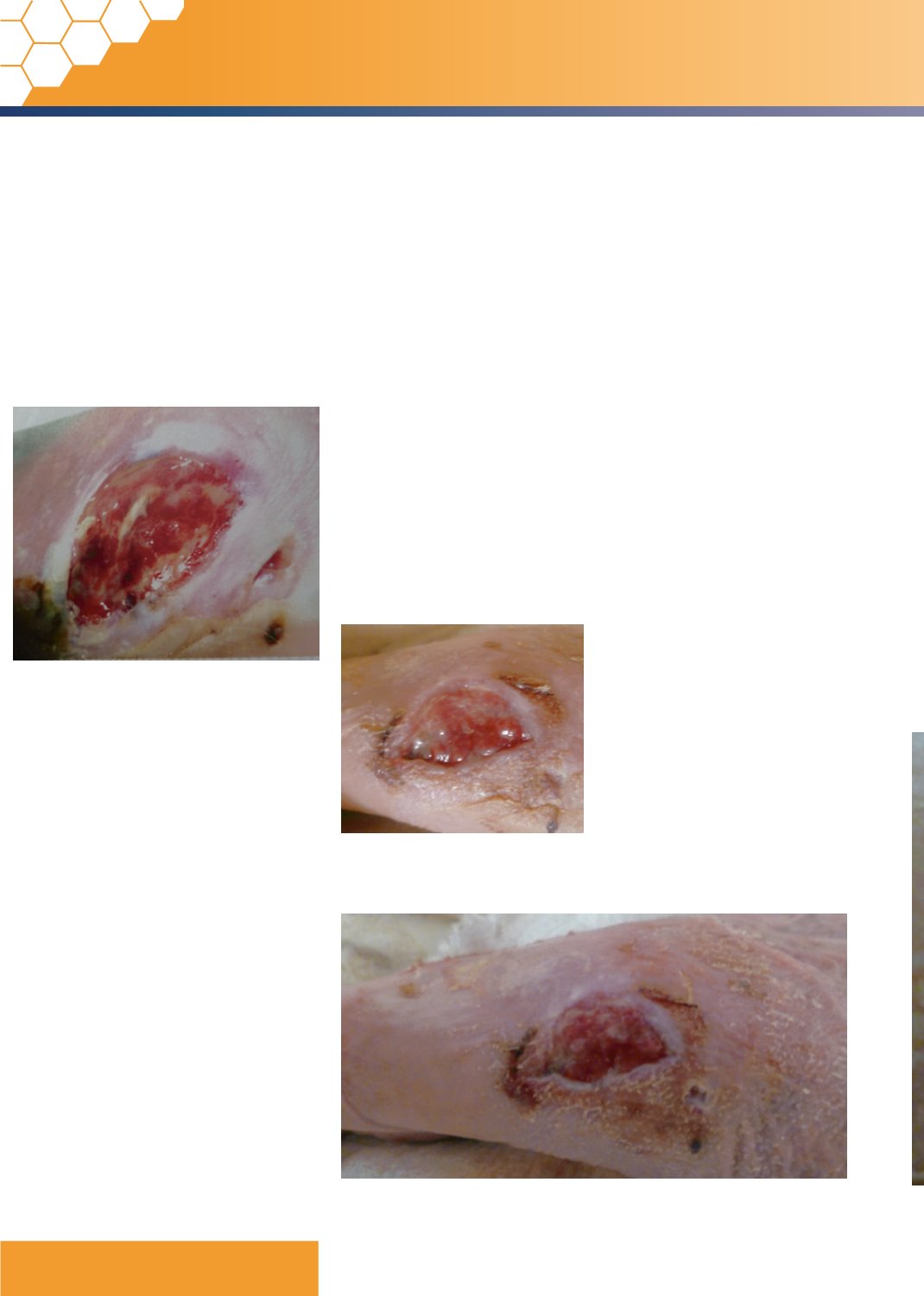
Figure 3.
The wound at week two, showing further granulation.
Figure 1.
Wound at week one showing 100%
granulation in the wound bed.
8
JCN supplement
2015,Vol 29, No 4