This patient was a 78-year-old female
non-smoker without any underlying
conditions, although her nutritional
status was described as poor. The
sacral abscesses had been present for
two weeks and were being dressed by
her regular nurses before she agreed
to join the Actilite Protect evaluation.
No systemic antibiotics were used
before or during the evaluation.
Wound progress
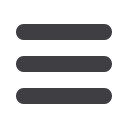
At presentation, the patient had two
sacral wounds, which were found to
be connected when probed (
Figure
1
). The wound bed comprised 100%
slough and the joint area of the two
wounds measured 4x3cm. There
were signs of local infection, the
periwound skin was reddened, and
the patient rated her pain as ‘8’ on
a scale of 1–10, where ‘10’was the
worst pain.
The dressings were being
changed every three days before
the switch to Actilite Protect. As
well as Actilite Protect (10x15cm),
the clinicians also applied
Sorbaderm
®
No-sting Barrier Film
CASE REPORT 4
This case features a patient
with two connected sacral
wounds that reduced in size
and severity when treated
with a honey-based
foam dressing.
(Aspen Medical) to the periwound
skin throughout the two-week
evaluation.
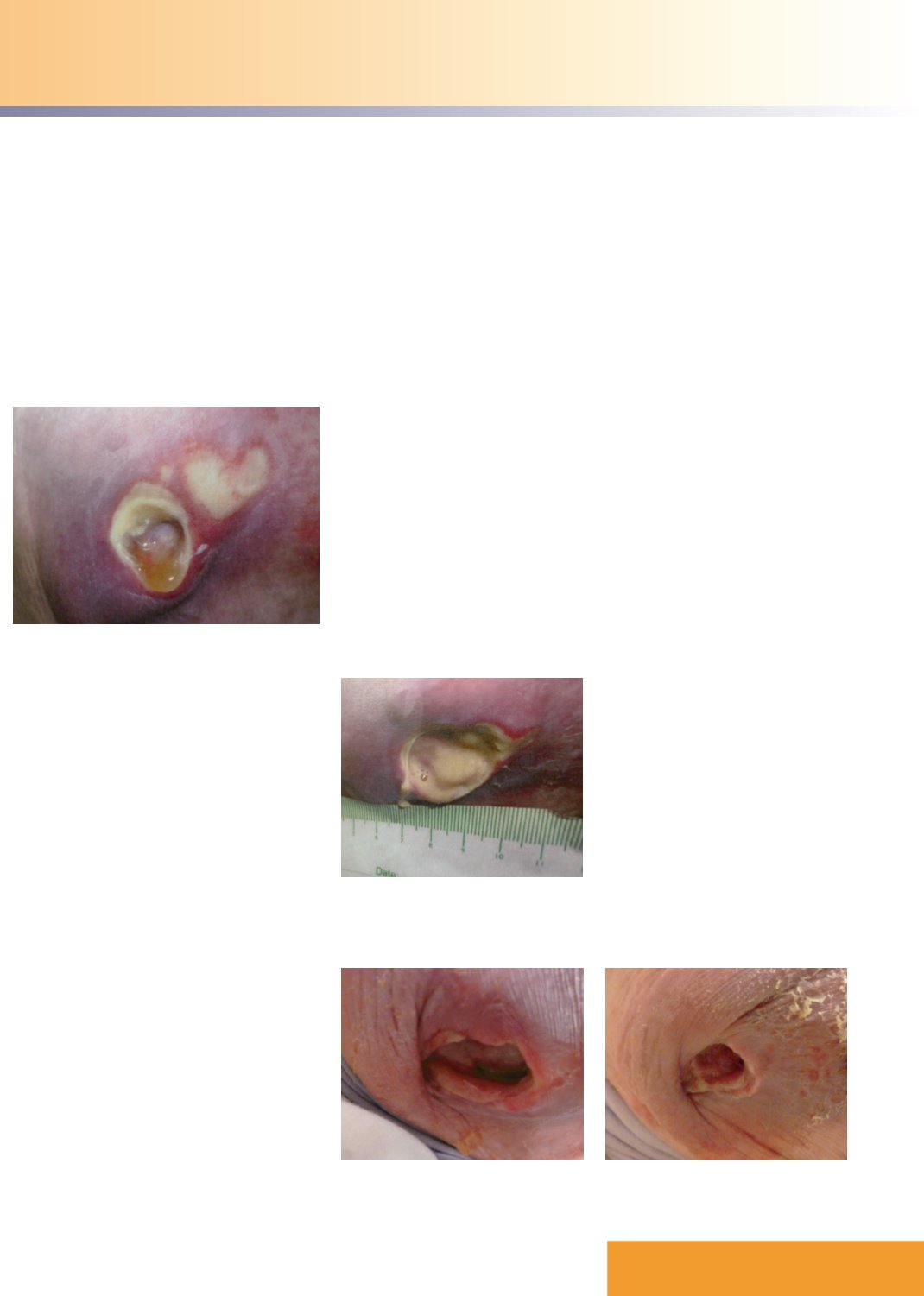
After a week of treatment with
dressing changes being performed
every three days, the wounds had
merged into one and the slough
had become ‘runny’ (
Figure 2
).
The overall wound dimensions
had not changed, there were
still signs of local infection and
the periwound skin was still red.
However, the pain was much
reduced and the patient now rated
it as ‘2’ on the 10-point scale.
By the end of the second week the
wound’s dimensions remained the
same but the wound bed comprised
100% granulation tissue and the
redness of the periwound skin was
greatly reduced
(Figure 3)
. There were
no signs of infection and the patient’s
pain levels had reduced to ‘0’.
The clinicians chose to carry on
using Actilite Protect even after the
evaluation was completed because it
had worked so well at reducing the
inflammation (
Figure 4
).
At the end of the evaluation
period the clinician was asked to rate
Actilite Protect on a scale of ‘1’ (very
easy) to ‘5’ (very difficult), and gave
it a score of 1. As well as being rated
easy to use and apply and very easy
to remove, the clinician also noted
that Actilite Protect was atraumatic
to the wound bed throughout the
dressing’s wear time. With regard to
conforming well to the wound, the
clinician rated it ‘3’ out of ‘5’, as it was
found to fit the shape of the patient’s
body well.
The patient did not experience
any pain due to the use of Actilite
Protect — this was also true of
removal, with no analgesia being
required. The dressing remained
intact on removal and stayed in place
while in use with no sign of rolling.
The clinician stated that Actilite
Protect’s dissolvable film of Manuka
honey made a great difference to
the condition of the periwound skin,
helping to reduce inflammation as
well as contributing to the healing
of the wound itself. The clinician
also appreciated the dressing’s
three-in-one action (foam, Manuka
honey and a silicone wound contact
layer), as this made dressing changes
easier. The patient reported that the
dressing was very comfortable. She
had experienced no pain from the
wound once the inflammation had
reduced and she was very satisfied
with the treatment.
Figure 1.
The connected wounds at presentation.
Figure 2.
After one week of treatment with Actilite
Protect, the two wounds had merged and
the slough had become ‘runny’.
Figure 3.
At the end of week two there was 100%
granulation in the wound bed.
Figure 4.
During the trial the inflammation was
greatly reduced.
JCN supplement
2015,Vol 29, No 4
7