JCN
Supplement 2016
9
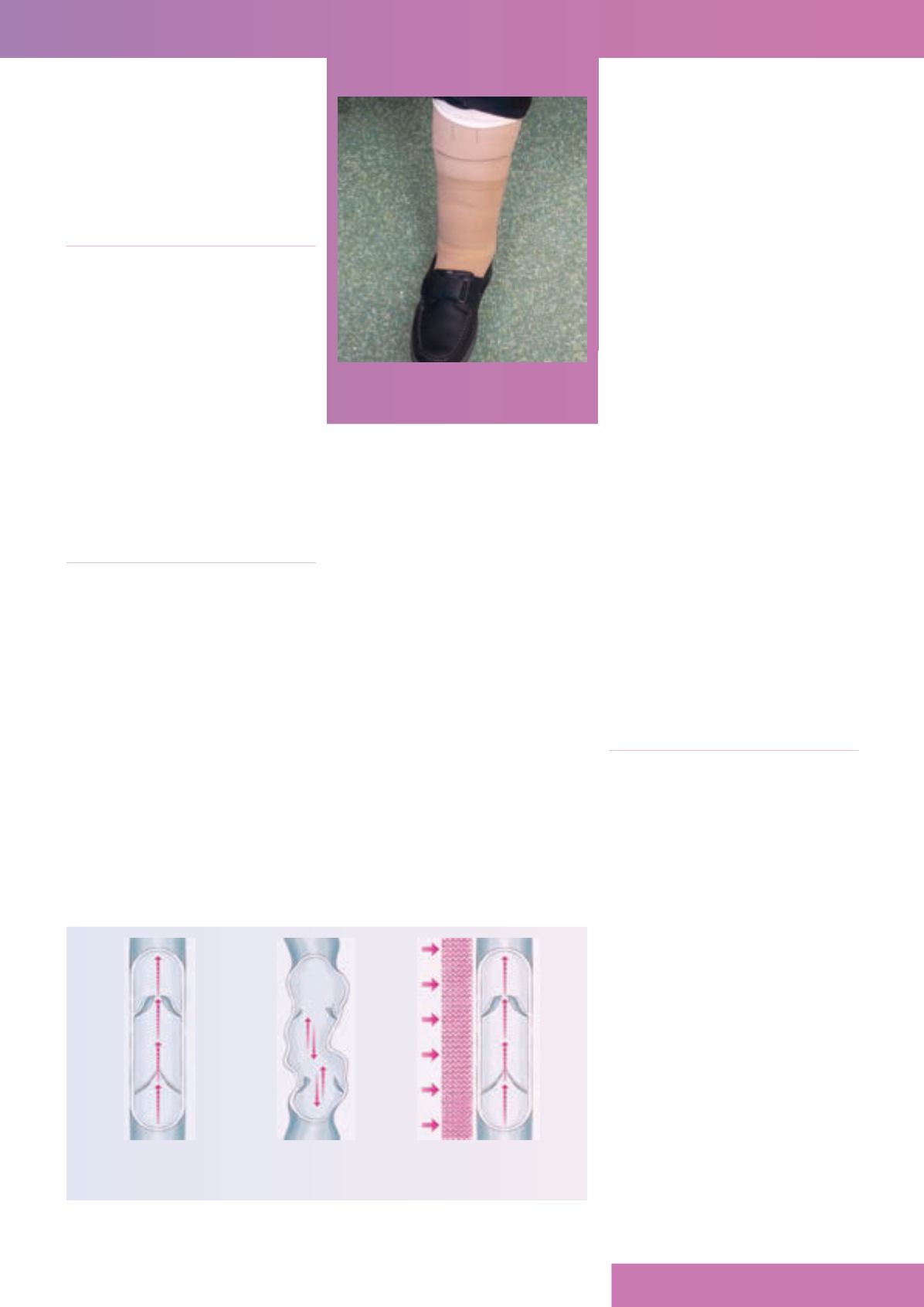
and gradually reducing higher up the
leg (i.e. 100% of compression is at the
ankle, reducing to 70% at the knee and
40% at the top of the thigh). The walls of
the compression garment improve the
function of the venous system (
Figure 1
).
COMPRESSION FOR PREVENTION
There is a wide range of compression
hosiery for patients with healedVLUs.
For example, mediven
®
RAL (medi
UK) range is available in different sizes,
both open- and closed-toe. It is readily
available on prescription (FP10/GP10),
reducing the need for made-to-measure
hosiery for many patients. mediven
active
®
has a soft fleecy sole making it
comfortable to walk in, while mediven
plus
®
offers a range of sizes that can
help improve the lipodermatosclerosed
limb shape often found in CVI.
AN ALTERNATIVE TO BANDAGING
WHERE HOSIERY IS UNSUITABLE
There are patients who have to be
maintained long term in bandaging
because they simply cannot apply or
tolerate compression hosiery. This
could be due to musculoskeletal
conditions hindering dexterity, or other
comorbidities that prevent them from
applying or removing compression
garments. Therefore, it is important
that general practice nurses (GPNs) are
aware of alternative systems that might
be more effective in helping patients to
prevent any ulcer recurrence and keep
their skin intact.
An example of such a device is
juxtalite
™
(medi UK). This is an inelastic
wraparound compression system. It
is easy to apply and adjust and allows
an immediate return to conventional
footwear. The device has a Built-in
Pressure System (BPS
™
), a method
by which the pressure applied can be
measured (at initial fit) and monitored
during the day. The calibrated card is
held against two lines on each strap and
the scale shows the mmHg applied. This
makes application a simple and safe
routine, and ensures that the wearer has
the optimal compression to deal with
the underlying disease and prevent
ulcers recurring.
juxtalite provides high working and
low resting pressure, ensuring comfort
for the wearer. The garment straps can
be instantly readjusted while on the
limb. With its latex-free properties,
anti-odour and antimicrobial fabric, it is
patient-friendly and gives sustained and
specifically defined compression for up
to 24 hours a day. It is available in eight
off-the-shelf sizes and two lengths.
It is comfortable and light to wear
and can be easily applied and removed
by the patient. It is also washable, and
can be dried in a tumble drier and is
guaranteed for six months’wear.
Converting from compression
bandaging to juxtalite can also help to
improve quality of life, as patients are
able to wear their own shoes again,
and, in the author’s clinical experience,
feel more independent as they are no
longer restricted by having to wait in
for nurse visits to have their bandages
changed, or to don/doff hosiery.
Anecdotal evidence shows that skin
condition improves — with juxtalite
being easy to apply and remove,
cleansing regimens can become regular
again with frequent applications of
emollients to improve skin hydration.
juxtalite not only offers an affordable
and acceptable choice, but also allows
sustained and measurable compression
to be worn to preventVLU recurrence
and enables patients to be involved in
their own care.
To cite this article:
Smith M (2016)
Appropriate compression is necessary to
prevent recurrence in venous leg ulceration.
J General Practice Nurs
2(4):
24–5
REFERENCES
Adderley UJ,Thompson C (2014) Community
nurses’judgement for the management
of venous leg ulceration: a judgement
analysis.
Int J Nurs Stud
52(1):
345–54
Harding K, Dowsett C, Fias L, et al (2015)
Simplifying venous leg ulcer management.
Consensus recommendations
. Wounds
International 2015. Available online: www.
woundsinternational
Jull AB, Mitchell N, Arroll J, et al (2004)
Factors influencing concordance with
compression stockings after venous leg
ulcer healing.
J Wound Care
13:
90–2
National Institute for Health and Care
Excellence (2016)
Leg ulcer — venous
. CKS.
NICE, London. Available online:
http://cks.nice.org.uk/leg-ulcer-venous
Nelson EA, Bell-Syer SEM (2012)
Compression for preventing recurrence
of venous ulcers.
Cochrane Database of
Systematic Reviews
: CD002303
Scottish Intercollegiate Guidelines Network
(2010)
Management of chronic venous leg
ulcers
. SIGN, Edinburgh
Shenoy M (2014) Prevention of leg ulcer
recurrence.
Ind Dermatol Online J
5(3):
386–9
JCN
Figure 1.
Venous system.
Healthy venous valve Defective venous
valve without
compression hosiery
Defective venous
valve with
compression hosiery
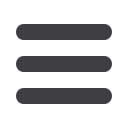
FIGURE 2.
juxtalite
in situ.









