
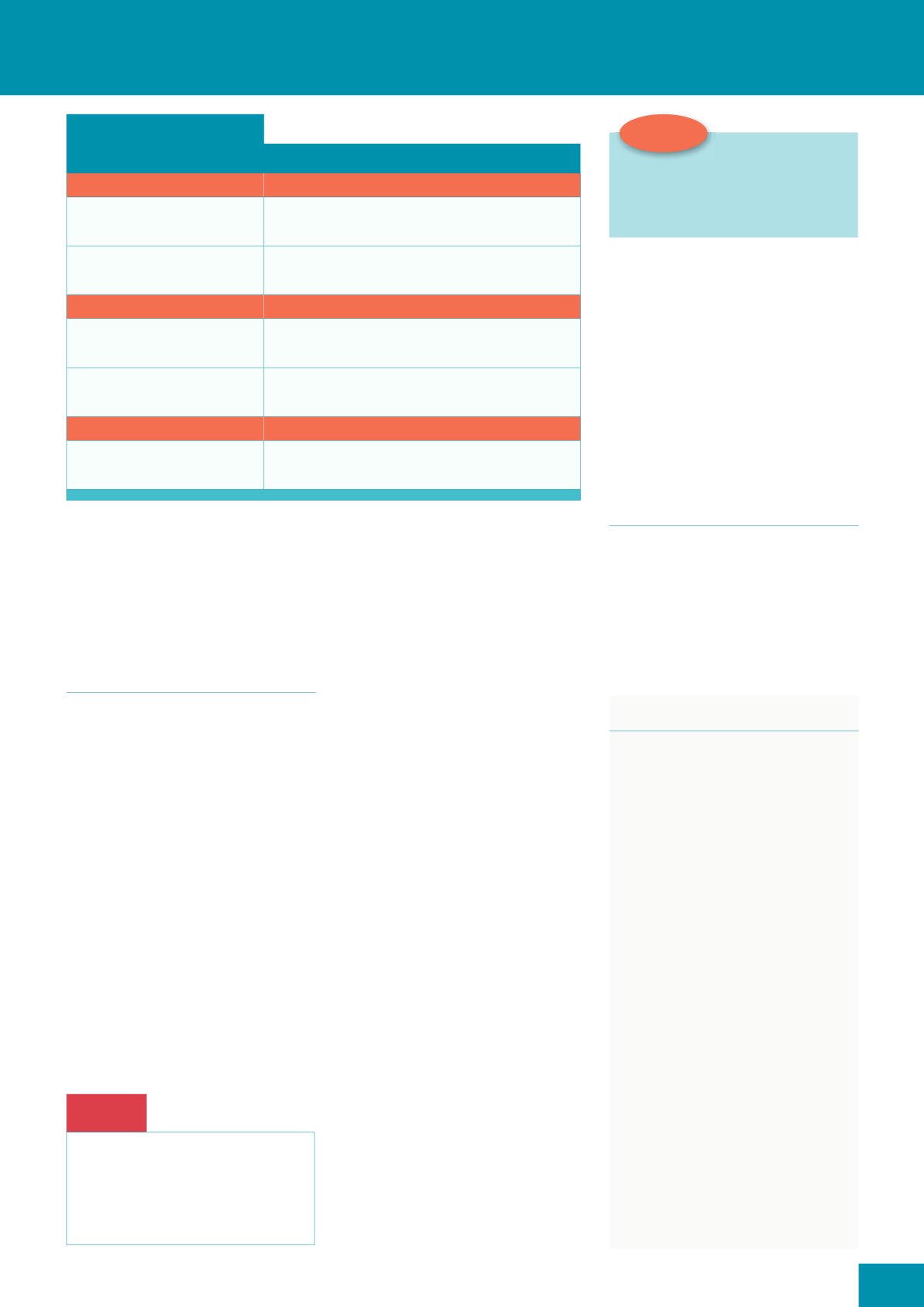
Box 1:
STAR classification system
Category 1: without tissue loss
Description
a. Linear
i
Edges can be realigned without stretching
i
Skin/flap is not pale, dusky or darkened
b. Linear
i
Edges can be realigned without stretching
i
Skin/flap is pale, dusky or darkened
Category 2: with partial tissue loss
Description
a. Less than 25%
i
Edges cannot be realigned
i
Skin/flap is not pale, dusky or darkened
b. More than 25%
i
Edges cannot be realigned
i
Skin/flap is pale, dusky or darkened
Category 3: with entire tissue loss
Description
i
A skin tear where the skin flap is totally absent
i
Refer to tissue viability team
SKIN TEARS AT A GLANCE
i
tissue (
Box 1;
Stephen-Haynes and
Greenwood, 2014).
In 2013, the International Skin
Tear Advisory Panel also introduced
a toolkit to prevent, assess and treat
skin tears (LeBlanc et al, 2013).
MANAGEMENT
This falls into four main stages
(Stephen-Haynes and Carville, 2011):
i
Cleansing the wound
i
Reapproximating the skin flap
i
Dressing the wound
i
Reviewing/reassessing.
Cleansing
Saline or running tap water should be
used to gently irrigate the wound and
remove any dirt/debris. The wound
should be carefully patted dry, not
rubbed, in order not to damage the
periwound skin.
Reapproximating the skin flap
If the skin flap is viable, gently ease it
back into position using tweezers or
gloved fingers and consider using this
skin as an improvised dressing.
Top tip:
Marking dressings with an arrow
to show the direction that they
should be removed will help to
OHVVHQ DQ\ ÁDS GLVWXUEDQFH
Red Flag
Always avoid using staples, sutures
and traditional adhesive strips
when reapproximating the skin
flap, as these may cause traction
and further trauma.
If it is difficult to align, use a
moistened swab for 5–10 minutes to
help rehydrate the area.
If the flap is large, wound closure
strips can be used on robust skin and
micro-adherent closure products on
fragile skin.
The surrounding skin should
always be protected with the use of a
barrier product.
Whichever method is used for
reapproximation, it should always be
documented in the patient’s notes.
Dressing the wound
To secure the flap, apply a non-
adherent or atraumatic dressing,
leaving a 2cm overlap. The condition
of the wound, i.e. the volume
of exudate being produced will
determine wear time, but it is
important to leave it in place for as
long as possible so as not to disturb
the flap.
Reviewing/reassessing
After 3–7 days, depending on the
condition of the wound, gently lift
the dressing, working away from the
skin flap. Silicone-based adhesive
removers can help to lessen any
trauma to the surrounding skin. It is
important to note the colour of the
skin flap, because if it is pale, dusky/
darkened it should be reassessed
within 24–48 hours to check for
any further skin breakdown. It is
also important to check for signs
of infection and, if present, treat
appropriately (European Wound
Management Association [EWMA],
2013). Again, always document
any changes.
If, however, the wound has
healed, stop dressings and instigate
a good skin cleansing regimen to
prevent recurrence.
CONCLUSION
Skin tears are common in the elderly.
However, prevention largely lies in
taking a commonsense approach
to identifying risks and following
a routine skin care regimen that
involves cleansing and moisturising
to maintain skin integrity.
REFERENCES
Battersby L (2009)
Nurs Times
105(16):
22–6
Beldon P (2006)
Wound Essentials
1:
108–9
Benbow M (2009)
J Community Nurs
23(1):
14–18
Carville K, Lewin G, Newall N, et al (2007)
Primary Intention
15(1):
18–28
EWMA (2013)
Antimicrobials and Non-
healing Wounds
. Available online: http://
ewma.org/fileadmin/user_upload/
EWMA.org/Project_Portfolio/EWMA_
Documents/Antimicrobial.pdf
LeBlanc K, Baranoski S (2011)
Adv Skin
Wound Care
24(9):
2–15
LeBlanc K, Baranoski S, Christensen D, et
al (2013)
Adv Skin Wound Care
26(10):
459–76
Payne RL, Martin ML (1993)
Ostomy
Wound Manage
39(5):
16–26
Stephen-Haynes J, Greenwood M (2014)
Wound Care Today
1(1):
58–64
Stephen-Haynes J (2012)
Br J Community
Nurs
Suppl March: S6, S8, S10
passim
Stephen-Haynes J, Carville K (2011)
Skin
Tears Made Easy.
Wounds International
SCT
SKIN CARE TODAY
2016,Vol 2, No 1
9









