
FOCUS ON PERIWOUND SKIN
i
12
SKIN CARE TODAY
2016,Vol 2, No 1
As a result, chronic wound exudate has
been referred to as a‘corrosive cocktail’
or‘toxic soup’and is very damaging to
the periwound area if not contained
within the dressing (Coutts et al, 2010).
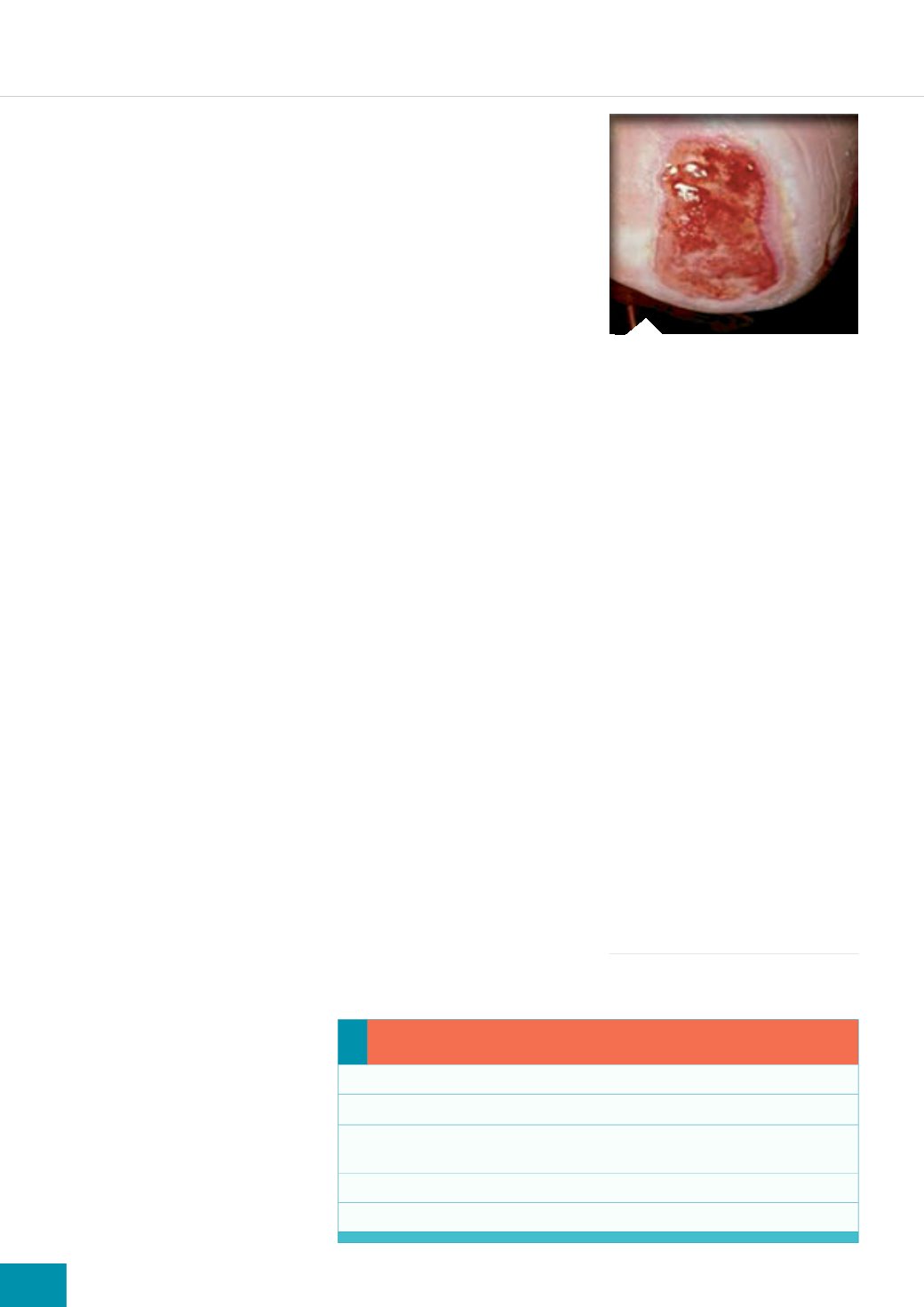
Maceration
Maceration develops when the wound
dressing is unable to handle the
volume of exudate, which, as a result,
overflows onto the surrounding skin
(
Figure 2
). It can be seen as a white
‘soggy’discolouration within four
centimetres of the wound edge and
develops as a result of overhydration
of the keratocytes in the skin and a
loss of epithelium (Cutting and White,
2002; Cameron, 2004; Thompson and
Stephen-Haynes, 2007).
A common‘everyday’ example of
maceration is that seen on the skin
after prolonged bathing, for example.
Macerated skin is weaker than non-
macerated skin and is easily damaged
by trauma and corrosive wound fluid
(Hollinworth, 2009). Macerated skin
also has a higher pH than normal
skin and is therefore at increased
risk of bacterial and fungal infections
due to the humid conditions created
by dressings (Langoen and Bianchi,
2013). It is important that nurses
understand how to protect the
periwound skin by ensuring that the
moisture balance within the wound is
well managed. Otherwise, the wound
can deteriorate and increase in size
(Mudge et al, 2008).
Erythematous maceration
As a result of prolonged contact with
wound exudate, the periwound skin
may become red, inflamed and also
shows signs similar to irritant contact
dermatitis (Cameron, 2004; Schofield,
2013). The patient may also report
burning, stinging and itching around
the affected area and the application
of a topical corticosteroid may be
needed for a few days to dampen the
inflammatory response before using a
skin protectant (Cameron, 2004). The
potency of the steroid is dependent
on the severity of the condition and
as the area improves, the potency and
frequency of application should be
reduced accordingly. Nurses should
apply any topical steroid sparingly
to the periwound area, taking care
that it is not in direct contact with
the wound, as this has been found to
delay healing (Marks et al, 1983).
Skin stripping
The repeated action of removing
and applying adhesive tapes and
dressings to the wound site will
eventually result in stripping of the
stratum corneum, the outermost
layer of the epidermis responsible
for maintaining the skin’s integrity
and barrier function (Langoen and
Bianchi, 2013).
Certain dressing types, such as
hydrocolloids, films and tapes made
of traditional adhesives are best
avoided in patients with very fragile,
vulnerable skin (Cutting, 2008).
Extra care should be taken when
treating patients who are undergoing
radiotherapy, which can render the
skin particularly vulnerable to trauma
(Goldberg and Mcgynn-Byer, 2000;
Hollinworth, 2009).
There are adhesive removal
products available on the market
that are designed to reduce the
trauma of dressing removal. Some
of these products contain silicone,
which helps to minimise the pain
and trauma of skin stripping. These
products are particularly useful
for patients with very fragile skin,
patients with epidermolysis bullosa,
or patients who experience painful
dressing changes (Stephen-Haynes,
2008). Some nurses have been known
to cut the adhesive border from
dressings before applying them as a
pragmatic solution to the problem of
protecting the fragile periwound skin
(Stephen-Haynes, 2008).
However, this is not
recommended since the dressing
will still need to be retained in
position and as Hollinworth (2009)
notes, using adhesive tape or other
film dressings to secure the primary
dressing will merely result in damage
to another area of skin.
Incorrect removal of wound
dressings can also result in skin
stripping. As a general rule, when
removing a dressing, the surrounding
skin should be supported by one
hand and the dressing gently lifted
off with the other hand; loosening
the edges first may also help and
some nurses find applying water
to the dressing edges to break
the adhesive bond helps this
process. Another strategy may be
to encourage the patient to remove
the dressing themselves; this is
particularly helpful where dressing
changes are painful. However, if pain
and trauma on dressing removal
persist, the nurse may need to
consider using alternatives such as
silicone-containing dressings, which
are designed to come away more
easily from the skin (Cutting, 2008).
TREATMENT OPTIONS
Barrier products
Traditionally, protecting the periwound
Practice points...
Periwound skin should form part of a wound assessment.
Assess exudate levels before selecting a dressing product.
Be aware that exudate levels may vary; HCPs need to change the type of
dressing accordingly.
Consider the use of barrier products when exudate levels are high.
Change the dressings according to the recommended wear time.
Figure 2.
Maceration from a highly
exuding wound.









