
Skin tears are commonly seen in the elderly and very young, due to the fragile nature of the
skin in these patient populations. With an increasing number of people living to older ages, the
incidence of skin tears is also likely to increase. Healthcare professionals need to understand the
importance of identifying those at risk, as well as effectively assessing and managing skin tears.
Assessing and managing skin tears can
seem challenging...
8
SKIN CARE TODAY
2016,Vol 2, No 1
WHAT IS A SKIN TEAR?
Skin tears are traumatic wounds that
usually occur in the elderly or those
with fragile skin (Stephen-Haynes and
Greenwood, 2014). They can be:
›
Partial-thickness (where the
epidermis separates from
the dermis)
›
Full-thickness (where both the
epidermis and dermis separate
from underlying structures)
(LeBlanc and Baronoski, 2011).
WHERE AND WHY DO
THEY OCCUR?
Although they can occur anywhere
on the body, they are most commonly
located on the extremities, such as
the arms and lower leg, as well as the
dorsal surface of the hand.
They are usually caused by an
accidental bump/knock, or from
friction and shear forces, and often
occur during routine care procedures.
Thus, many are considered to
be preventable.
In the very young, they can be
caused by adhesives or as a result of
trauma from devices (LeBlanc and
Baranoski, 2011).
Risk factors
Identifying risk factors for skin tears
in each individual patient plays an
important part in prevention. These
can include:
›
Previous history of skin tears
›
Elderly or very young skin
›
Poor mobility
›
Inadequate nutrition/hydration
›
Cognitive/sensory impairment
›
Other underlying comorbidities,
i.e. chronic heart failure,
renal failure
›
Long-term steroid use
›
Highly dependent patients,
i.e. those who need help when
showering, etc
›
Dry, fragile skin, or skin that is in a
poor condition.
ASSESSMENT AND
CATEGORISATION
If a person has a skin tear, the first
step is to take a full patient history to
establish if this has occurred before.
The person’s underlying medical
condition and health status should
also be considered (Stephen-Haynes,
2012). Although the cause of a skin
tear cannot always be determined
(Benbow, 2009), if this is possible, e.g.
due to trauma or friction/shear forces,
this can help to ensure that measures
are put in place to prevent recurrence.
The skin around the tear should
also be examined, as this will help to
decide which dressings can be used.
For example, if the surrounding skin
is very fragile, a soft silicone-coated
dressing will help to stabilise the skin
flap without having to use adhesives
(Beldon, 2006).
It is also important to consider
SKIN TEARS AT A GLANCE
›
the patient’s nutritional status, any
medication that they might be on,
wound location and the size and
category of skin tear.
There is no one standard
classification system for skin tears.
However, using one helps both
with assessment and to guide the
treatment plan (Battersby, 2009). Two
commonly used systems are:
›
Payne-Martin, 1993
›
Skin Tear Audit Research (STAR)
(Carville et al, 2007).
Both systems identify three
different categories, but the STAR
system is more detailed with regard
to the amount of epidermal loss
and condition of the epidermal
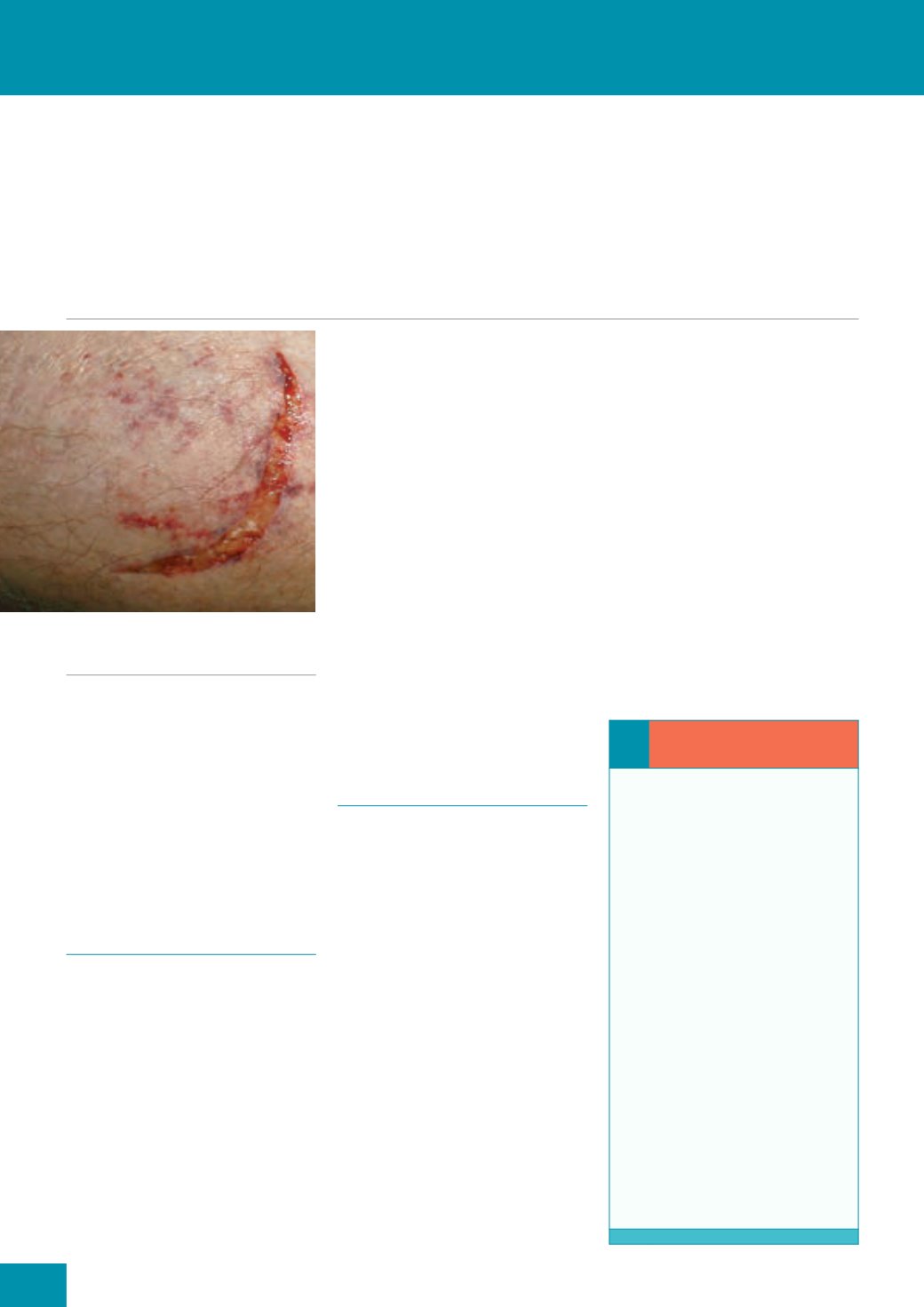
Figure 1.
A typical skin tear.
❛❛
Prevention: top tips...
Avoid wearing jewellery that
could ‘snag’ the skin
Keep nails short
Follow good manual-handling
techniques
Use appropriate aids to
transfer patients
Never apply adhesives directly
to the skin
Avoid soaps that dry the skin
Keep skin well hydrated
Ensure good lighting
Remove any small tables/chairs
that might be in the way
Cover any sharp corners of
furniture with soft materials
Advise patients to wear long
sleeves, trousers, or knee-high
socks, etc to protect fragile skin









