Differentiating between moisture- and pressure-related skin damage is notoriously difficult for
clinicians. Here Jacqui Fletcher, independent nurse consultant, looks at the differences between the
two types of skin damage, as well as focusing on how to prevent the development of moisture-
associated lesions.
Identifying the difference between moisture
lesions and pressure damage
8
SKIN CARE TODAY
2017,Vol 3, No 1
BACKGROUND
Moisture lesions have featured in
the literature for over ten years,
yet there remains considerable
confusion between these lesions
and pressure ulcers, with pressure
ulcer prevalence studies still
reporting that staff find it hard to
differentiate between the two types
of skin damage (Smith et al, 2016).
This is compounded by a lack of
consistent definitions and varying
terminology (
Box 1
); for example,
damage to the sacrum and buttocks
from exposure to urine is
commonly referred to as a
moisture lesion, but may also be
termed incontinence dermatitis,
incontinence-associated dermatitis
(IAD), or moisture-associated skin
damage (MASD) (Yates, 2012).
While MASD or moisture lesions
may be seen as umbrella terms
to encompass a range of other
indications (
Box 2
), a moisture
lesion is more commonly (but not
exclusively) found on the patient’s
‘bottom’, while MASD may occur
anywhere on the body.
There are two main frameworks
used to differentiate between
moisture and pressure damage.
The Pressure Ulcer Classification
(PUCLAS) tool, originally
described by Beeckman et al (2010),
addresses:
›
Cause
›
Location
›
Shape
›
Depth
›
Necrosis
›
Edges and colour.
On the other hand, Black et al’s
(2011) tool seeks to differentiate
between IAD and category one and
two pressure ulcers and looks at:
›
History
›
Location of affected skin
Box 1:
Definitions used within the literature
All Wales Tissue Viability Forum and All Wales Continence Forum (2012)
›
A moisture lesion is defined as being caused by urine and/or faeces and perspiration, which is in
continuous contact with the intact skin of the perineum, buttocks, groin, inner thighs, natal cleft and
skin folds, and where skin is in direct contact with skin. Moisture lesions cause superficial loss of
epidermis and/or dermis, which may be preceded by areas of erythema on intact skin. They will usually
cause pain. The skin will either be excoriated, which presents as superficial red and dry broken skin, or
macerated, presenting as red and white, wet, soggy, and shiny skin.
›
The pattern of skin damage is uneven apart from on the natal cleft when the damage presents as a linear
vertical split in the skin. In the case of so-called‘kissing’lesions, the damage usually presents on either
side of a skin fold.
Young (2012)
›
Young defines a moisture lesion as a reactive response of the skin to chronic exposure to urine and
faecal matter, which could be observed as inflammation and erythema, with or without erosion and
denudation. Typically, there is loss of the epidermis and the skin appears macerated, red, broken and
painful (Cooper et al, 2006; Gray et al, 2007).
Kottner and Halfens (2010)
›
Prolonged exposure of the skin to perspiration, urine, faeces or wound exudate may lead to irritation,
inflammation and erosion of the superficial skin layers.
Gray et al (2011)
›
Moisture-associated skin damage (MASD) is defined as inflammation and erosion of the skin caused
by prolonged exposure to various sources of moisture, including urine or stool, perspiration, wound
exudate, mucus, or saliva.
MOISTURE LESIONS AND PRESSURE ULCERS AT A GLANCE
›
›
Colour of wound bed
›
Colour of periwound tissue
›
Characteristics of involved area
›
Pain
›
Odour
›
Other.
It is also important to remember
that combined lesions can occur
where damage due to both pressure
and moisture are present.
Perhaps the most important
question is — what is the cause of
the damage? If there is no history
of moisture in an area affected by
pressure, then the wound is clearly
a pressure ulcer and visa versa.
While other factors such as location
are important they are less clear,
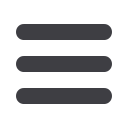
Figure 1.
Linear sloughy wound in the
patient’s natal cleft.