10
SKIN CARE TODAY
2017,Vol 3, No 1
MOISTURE LESIONS AND PRESSURE ULCERS AT A GLANCE
i
with both pressure and moisture
damage occurring commonly on the
sacrum, for example. A lesion that
occurs in the natal cleft between
the buttocks and is linear in shape
(
Figure 1
) is clearly moisture-related
and as it is located in a place where
moisture easily collects and is not
located over a bony prominence,
it is unlikely to be due to pressure
unless the patient has been sat on a
device such as a catheter.
PREVENTION AND
MANAGEMENT
Clinically, it is important to
differentiate between a pressure
ulcer and moisture lesions/MASD
as the prevention and management
plan will vary according to which
is being treated (Fletcher, 2008;
Kottner and Halfens, 2010).
When considering prevention
and management of either wound
type, the most important factor
is, where possible, to remove the
cause. For pressure ulcer prevention,
this involves improving mobility,
repositioning and the use of
specialist equipment; whereas for
moisture lesions, keeping the skin
clean, dry and well-moisturised
are key.
Top tip:
It is vital to differentiate between
a pressure ulcer and moisture
damage, as prevention and
management will vary according
to which is being treated.
Where it is not possible to fully
remove the cause, actions should be
taken to maximise the individual’s
potential to maintain healthy skin.
In both MASD and pressure ulcers,
this includes:
i
Regular skin inspections to
identify problems quickly
i
Keeping the skin clean, dry and
well-moisturised/hydrated.
Lichterfeld et al (2015)
developed an algorithm that
suggests skin care techniques
for managing incontinence and
preventing pressure ulcers. The
algorithm is simple to follow and
focuses on the care of dry or
humid skin, targeting different
areas of the body — trunk, scalp
and face, extremities and feet,
anogenital and interdigital, as
well as areas of ‘skin on skin’, e.g.
abdominal skin folds and the skin
underneath breasts.
Preventing moisture damage
A range of barrier products are
available to prevent moisture-
related skin damage. These provide
additional protection for the skin
and come in creams and sprays or
as part of a ‘3-in-1’ cloth (which
washes, moisturises and forms a
barrier on the skin’s surface).
The use of ordinary soap and
water should be avoided in patients
with vulnerable skin, as in most
cases the pH of the soap is too
alkaline, and may contribute to any
irritation (Voegeli, 2010; Lichterfeld
et al, 2015). However, skin care
product selection can be difficult
due to heterogeneous labelling and
claims about performance, therefore
local guidance should be followed.
Where moisture-related skin
damage does occur, it must be
remembered that this in turn
increases the susceptibility of the
patient to pressure damage as it
renders the skin more vulnerable
to shear, friction and mechanical
stripping, as well as to pressure
itself (Black et al, 2011). For
example, extra care should be
taken, particularly with moving
and handling, to ensure that the
patient’s skin is not dragged along
the surface of beds and chairs as
this can result in shear forces and
deep tissue damage.
CONCLUSION
Identifying the type of skin damage a
patient is at risk of is important as it
affects the care that will be delivered.
In reality, many patients are at risk
of both pressure ulcers and moisture
lesions and care should be planned
to ensure that activities meant to
prevent one do not increase the risk
of the other, such as using too many
pads to manage incontinence which
may block the action of a pressure-
redistributing mattress.
Once a lesion occurs, it is
important to get the diagnosis
correct, both to ensure the patient
receives appropriate care, and
also, from an organisational point
of view, to ensure that the skin
damage is accurately reported.
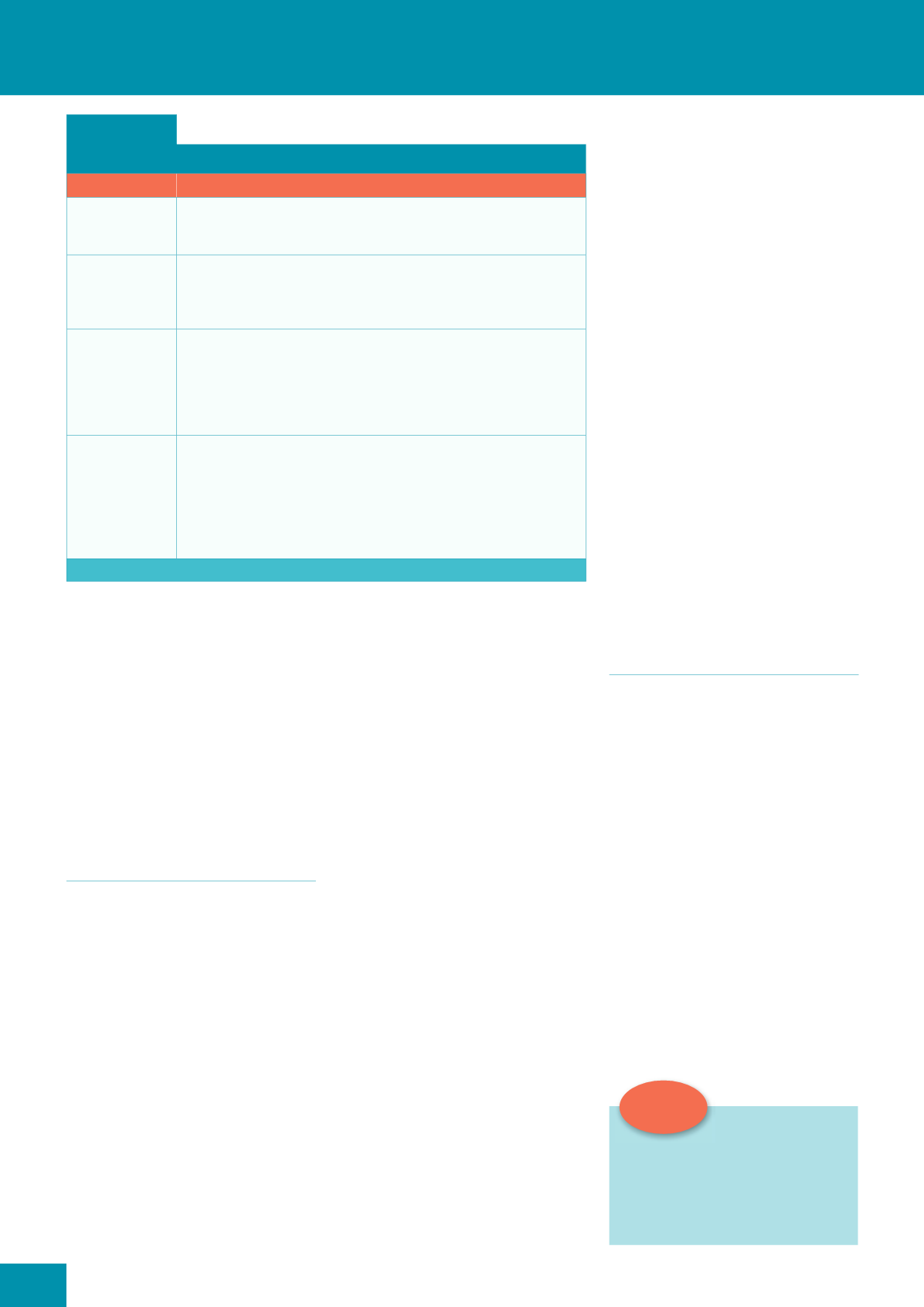
Box 2:
Types of moisture-associated skin damage (MASD)
Type of MASD
'HÀQLWLRQ FKDUDFWHULVWLFV
Incontinence-
associated
dermatitis (IAD)
Prolonged contact with the skin of urine or faeces is also known as IAD. Typically, it
presents as inflammation of the skin’s surface characterised by redness, and in some
cases, swelling and blister formation (Voegeli, 2012).
Peristomal
moisture-
associated
dermatitis
Inflammation and erosion of skin, related to moisture, that begins at the stoma/skin
junction and can extend outwards to a four-inch (10cm) radius.
Periwound
moisture-
associated
dermatitis
When a high volume of exudate is produced, healing may be affected as the
overhydrated skin becomes macerated, potentially leading to skin breakdown
(Cutting, 1999). Exudate from acute wounds contains proteolytic enzymes that tend
to be inactive. In contrast, chronic wounds have a higher amount of proteolytic
enzymes, which tend to be more active and predispose skin to breakdown (Colwell
et al, 2011).
Intertriginous
dermatitis
An inflammatory skin condition that affects opposing skin surfaces commonly
found in the axillary and inguinal skin folds, as well as under the breasts in females
(Black et al, 2011). Thought to be caused by friction that occurs when the skin
rubs together and is worsened by trapped moisture, which is a result of poor air
circulation (Black et al, 2011). Leads to mild erythema and may progress to more
serious inflammation with erosion, oozing, exudation, maceration and secondary
infection (Hahler, 2006).
SCT