52
WOUND CARE TODAY
2017,Vol 4, No 1
FOCUS ON
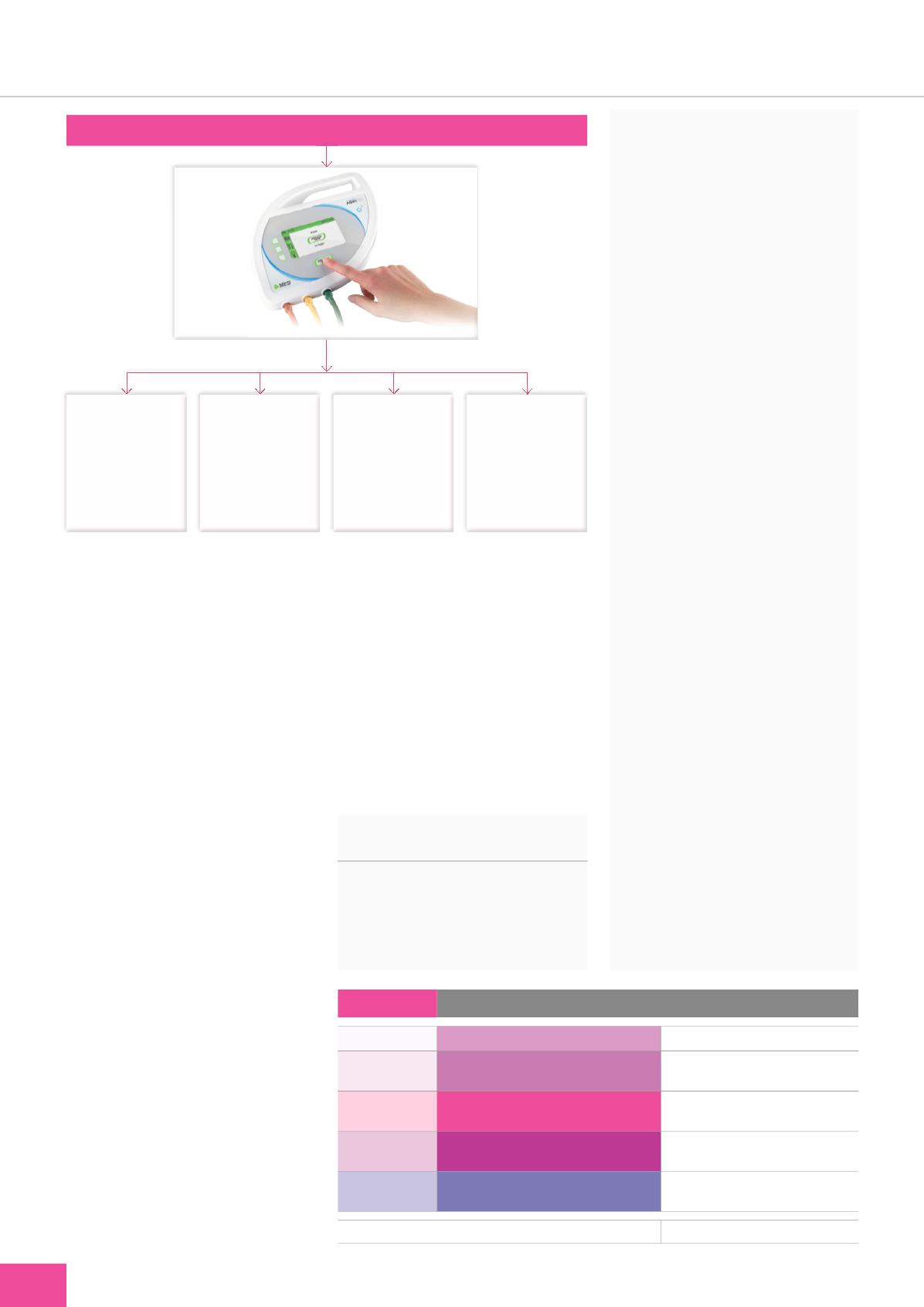
ABPI
i
is less than 0.8 but greater than 0.5,
reduced or modified compression can
be applied with specialist supervision
or guidance (
Figure 1
).
Leg ulcer assessment should be
ongoing until a wound has healed,
including regular measuring of a
patient’s ABPI. Furthermore, after
healing has occurred and the patient
has been fitted with maintenance
compression garments to prevent
recurrence, ABPI recordings should
continue to be taken at regular
intervals. The Royal College of
Nursing (RCN, 2006) guidelines
suggest three monthly reviews,
including ABPI. A recent Best Practice
Statement (Wounds UK, 2016)
suggested that patients should be
reassessed at three, six or 12 monthly
intervals, depending on patient
needs, initial assessment outcome
and cardiovascular risk factors, or
in line with local guidance. This will
confirm that there are no alterations
in arterial status and that patients
remain suitable for compression
therapy. Any deterioration identified
should be referred to specialist
services as soon as possible.
A simple way of measuring
ABPI with no need for resting the
patient beforehand, as required
with traditional Doppler devices, is
Patient with leg or foot wound, or in need of compression therapy
MESI ABPI
MD
<0.5: urgent referal to
vascular specialist.
Severe arterial disease,
compression is
contraindicated
0.5–0.8: mixed atielogy
reduced compression
may be suitable in
these cases under
specialist supervision,
e.g. juxta measurable
compression set
at 20mmhg
0.8–1.3: venous ulcer
suitable for full
compression of
40mmHg, e.g.
juxta measurable
compression set
at 40mmhg
>1.4 indicates
incompressable arteries
for onward referal to
vascular specialist for
further investigation
Table 1:
ABPI indicators for compression therapy
ABPI > 1.0–1.3
No indicators of peripheral vascular disease
Apply high levels of compression therapy
ABPI = 0.81–1.0
Mild peripheral disease
May have high levels of compression
therapy — monitor ABPI
ABPI = 0.51–0.8
Significant arterial disease
May have reduced compression — refer
to specialist nurse/vascular specialist
ABPI = < 0.5
Severe arterial disease
No compression — urgent referral
to vascular specialist
ABPI > 1.3
Measure toe pressures or refer to specialist
May have compression therapy — liaise
with specialist nurse/vascular specialist
Young patients may have high ABPI not indicative of PAD (8)
(Adapted from Harding et al, 2015)
Figure 1.
ABPI results and appropriate treatment
.
Beldon P (2011) Ten top tips for Doppler
ABPI.
Wounds Int
2(4):
18–21
Chamanga E, Christie J, McKeown E
(2014) Community nurses’experiences
of treating patients with leg ulcers.
J
Community Nurs
28(6):
27–34
Fox C (2003) The holistic assessment
of a patient with leg ulceration.
Br J
Community Nurs
8(Supp126):
S30
Guest JF, Ayoub N, McIlwraith T, et al
(2015) Health economic burden that
wounds impose on the National Health
Service in the UK.
BMJ Open
. Available
online:
http://bmjopen.bmj.com/content/5/12/e009283
Harding K, Dowsett C, Fias L, et
al (2015) Simplifying venous leg
ulcer management. Consensus
recommendations.
Wounds
International
. Available online:
www. woundsinternational.com/con sensus- documents/view/simplifying-venous- leg-ulcer-managementNHS England (2016)
CQUIN 2017–19
Guidance
. Available online:
www. england.nhs.uk/nhs-standard-contract/cquin/cquin-17-19/
Royal College of Nursing (2006)
The
management of patients with venous leg
ulcers
. Clinical practice guidelines.
RCN, London
Scottish Intercollegiate Guidelines
Network (2010)
Management of venous
leg ulcers. Clinical guideline no.120
.
SIGN, Edinburgh. Available online:
www.sign.ac.ukWorboys F (2006) How to obtain a resting
ABPI in leg ulcer management.
Wounds
Essentials
1:
55–60
Wounds UK (2016)
Best Practice Statement:
Holistic management of venous leg
ulceration
. Wounds UK, London
using the MESI ABPI MD (available
from medi UK;
Figure 1
). A simple
start button is pressed after placing
cuffs, which simultaneously inflate
and deflate to give an accurate ABPI
reading, along with blood pressure
(BP)/pulse and waveforms within one
minute. The device is also portable
and powered with a lightweight
battery, making it a safe and
useful tool for any community
nurse’s armamentarium.
REFERENCES
Adderley JU, Thompson C (2015)
Community nurses’judgement for the
management of venous leg ulcerations:
a judgement analysis.
Int J Nurs Stud
52(1):
345–54
WCT