16 JCN supplement
2018,Vol 32, No 2
WOUND ASSESSMENT CQUIN
`
Quarter three — establish targets
for improvement and
educate practitioners
`
Quarter four — re-audit.
Year two targets will be
set nationally based on the
data submitted.
To establish baseline data at
the author’s trust, all wound care
templates completed in the last year
were collated by information services
fromApril 2016 until March 2017. All
patients who had a chronic wound
(defined as one present for more than
four weeks), including pressure, leg,
and diabetic foot ulcers, or surgical
dehisced wounds were included in
the sample. To create a sample of
151 patients, they were collated into
wound type, with percentages of each
wound type being used to generate
a representative sample. Based on
this calculation, a random sample of
each type was audited against the
standards set out in the minimum
dataset (random selection was based
on the total number of wounds per
category divided by the number of
responses needed, which generated
the frequency of selection from the
list of patients) by the tissue viability
team. Unfortunately, records had to
be hand searched as SystmOne was
used and not all the minimum dataset
has associated read codes. This made
creating a computer-generated report
impossible. Data was gathered using
a spreadsheet and a report generated
from analysing that data.
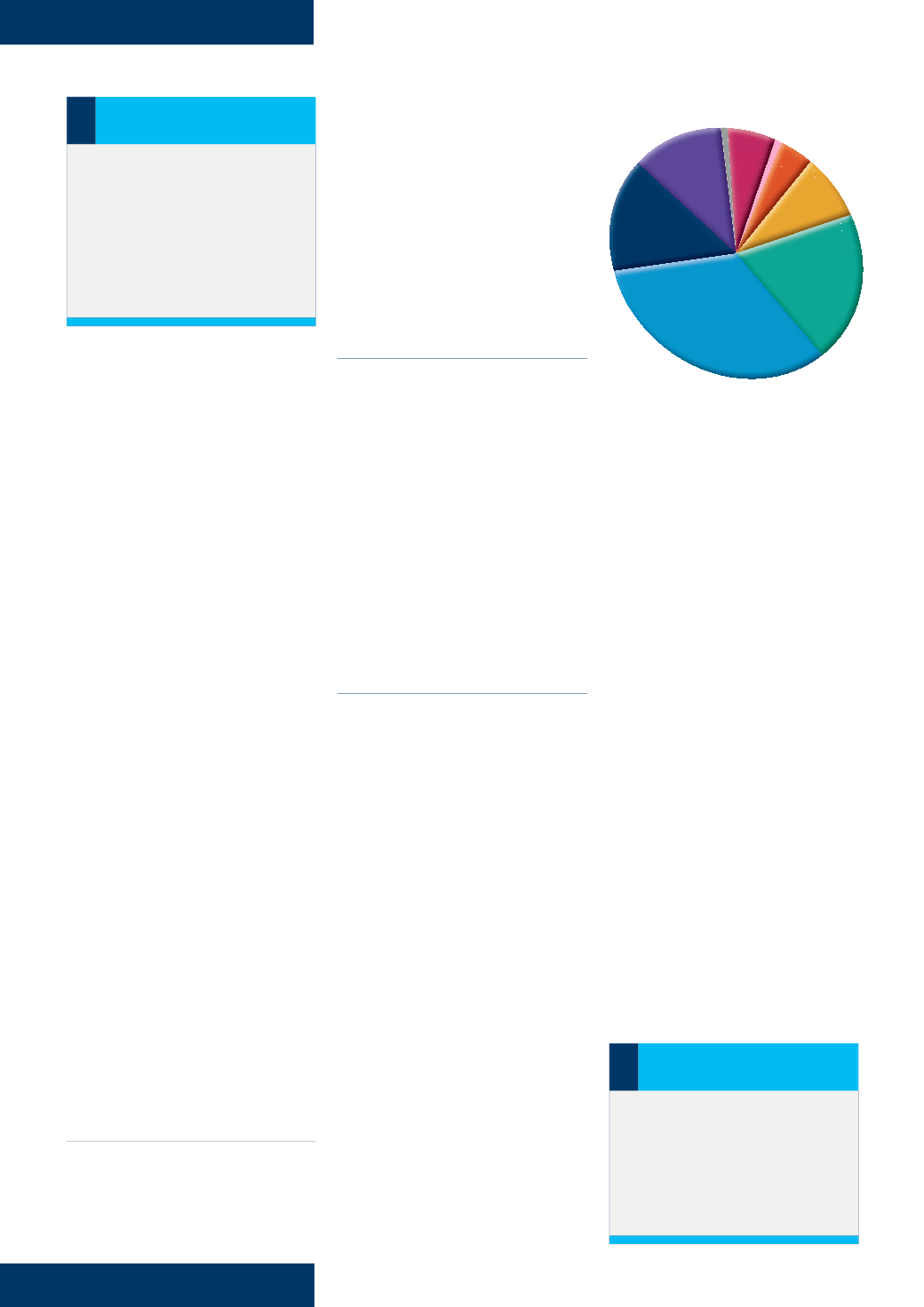
DEMOGRAPHICS
The demographic analysis revealed
slightly more female (78) than male
(73) records. Before data analysis,
the team had expected more female
patients, as women have a higher life
expectancy than men, however well
matched. The age of patients ranged
from 17–97, with the average age
being 70 years old — a median age
of 72 years, with 58% of the sample
being over the age of 70 years (
Figure
1
). This was despite a backdrop of an
average healthy life expectancy for
patients living in the catchment area
of 59.6 years, which is more than four
years less than the national average
(North Tyneside CCG, 2017).
PLACE OF RESIDENCE
Most patients were living in their own
homes (139; 92%), with the remainder
in residential care (12; 8%). Ninety-
six (63.6%) patients received care in
their normal place of residence, the
remaining 55 (36.4%) in a community
clinic setting. It can be assumed that
the patients receiving care in clinics
were less frail than the housebound
patients and that they did not meet
the organisation’s criteria for home
visits. However, no subset analysis
of this patient group was made, and
this represents a limitation of the
data presented.
CHRONICITY FACTORS
A high number of patients presented
with chronicity factors associated in
the literature with delayed wound
healing (Anderson and Hamm,
2012). One in five of the patients in
the sample had been assessed by a
SystmOne user as having vascular
insufficiency, more specifically
peripheral arterial disease (PAD). Only
one-third of the patients had their
smoking status assessed by the team
caring for them. This can be linked
to high rates of smoking-related
admissions to hospital; the area sees
almost 250,000 per year — this is
50% higher than the national average
(North Tyneside CCG, 2017).
Of the sample, 14 patients
had diabetes and 25 patients had
entries in their record in relation to
having at least one other chronic
illness, such as multiple sclerosis or
rheumatoid arthritis, which, when
coupled with the diabetes responses,
is over a quarter of the sample.
Additionally, 37 of the patients had
been screened for malnutrition and
were considered to have assessment
scores which warranted intervention
or monitoring; and 17 patients in
the sample were categorised as
obese. A quarter of the sample had
entries that related to immobility and
incontinence, and a further 28 of the
patients had been formally assessed
for frailty, which represented a
staggering 43% of the sample. Of the
remaining patients, 11 were taking
medications that affected healing and
seven patients with diabetes were
recorded as having neuropathy. A
third of the patients in the sample
had had a previous wound (range
1–8), the most common frequency
being one previous wound.
Wound recurrence is also linked
with chronicity and difficulties in
achieving healing, and could be
viewed as a failure to influence patient
behaviours that affect recurrence, such
as wearing hosiery in the leg ulcer
group or offloading for the diabetic
foot (Frykberg and Banks, 2015). Other
patients in each wound type group had
no entry of having been assessed for
provision of hosiery or offloading, but
absence of data cannot be assumed
to mean that the condition had been
assessed and was absent. The data was
not present in the records.
Figure 1.
Age distribution of patients.
i
What is CQUIN
CQUIN is an acronym for
Commissioning for Quality and
Improvement. This system aims to
make a proportion of a healthcare
provider’s income dependent upon
their demonstrating quality and
improvement in an agreed area
of care.
90+
80–89
70–79
60–69
50–59
40–49
20–29
17
30–39
i
PRACTICE POINT
CQUINs focus on three areas
of quality where innovation should
be seen:
`
Safety
`
Effectiveness
`
Patient experience.