JCN supplement
2014,Vol 28, No 5
7
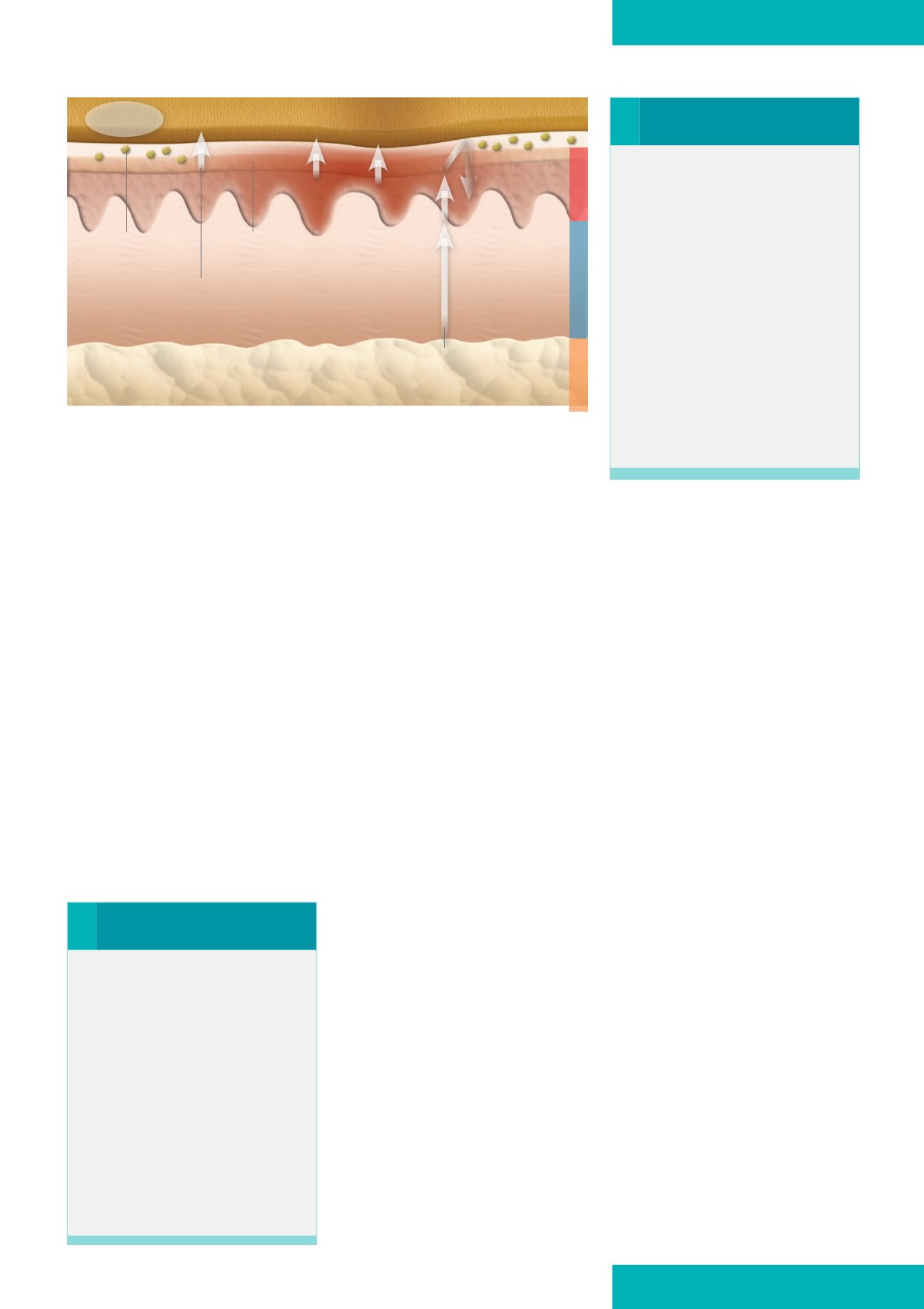
MEDICAL GRADE HONEY
The autolytic debriding action
of honey comes from its ability to
convert inactive plasminogen in the
wound matrix to the active enzyme,
plasmin (Molan, 2005). Honey
helps debridement by creating an
ideal moist wound environment to
facilitate autolysis by drawing out
lymph fluid from the wound tissues
through its strong osmotic action
(
Figure 1
). This osmotic action also
rehydrates devitalised tissue (Gethin
and Cowman, 2008). This offers a
plentiful supply of plasminogen
to the interface of the wound bed
and overlying slough, washing the
surface of the wound bed from
beneath. The activation of proteases
by H
2
O
2
also offers an explanation
for the rapid debridement observed
when honey is used (White and
Molan, 2005). The debriding action
of honey can be faster than other
dressings (Molan, 2005).
Angiogenesis is stimulated due to
honey’s anti-inflammatory effect,
which results in decreased oedema
and a consequent decrease of
pressure on capillaries allowing for
improved blood flow and supply of
oxygen to the regenerating wound
tissues. Alongside this action, honey
stimulates the growth of fibroblasts
which are essential components in
supporting normal wound healing
(Bainbridge, 2013).
Other actions of honey which effect the
stimulation of new tissues
Hydrogen peroxide produced enhances
cutaneous blood flow in ischaemic
tissues and the stimulation of new
tissue growth, which normally starts
the healing process (Molan, 2005).
Biofilms
The antimicrobial action of honey
cannot be discussed without also
considering its action on biofilms.
Growing evidence supports the
recognised link between the presence
of biofilms in a wound to chronicity
(Merckoll et al, 2009) and impeded
wound healing (Phillips et al, 2010).
Research has found that honey can
prevent biofilm formation and in
higher concentrations has the ability
to break down established biofilms
(Seckam and Cooper, 2013).
Pain management
Literature suggests that the use of
honey wound dressings may be
painful due to acidity (Alswayeh and
Anti-inflammatory action
Inflammation is a normal response
to injury or infection and makes up
the early stages of wound healing
(Hutchinson, 1992). A prolonged
inflammatory reaction can inhibit
healing, cause hypertrophic scarring,
prolong discomfort, increase exudate
and formulate chronic hard-to-
heal wounds (Stephen-Haynes and
Callaghan, 2011).The mechanism
by which honey reduces excessive
inflammation is not clearly understood.
It has been suggested that it may be
linked to the high levels of antioxidants
contained in honey‘mopping up’free
radicals (Molan, 2005).
Scar reduction
The potent anti-inflammatory action
created by honey appears to have
no known adverse effects on cells
and actually has the potential to
stimulate tissue growth. The anti-
inflammatory action of medical grade
honey can reduce some scarring
and contractions (Subrahmanyam,
2001). One explanation for this is
that a prolonged inflammation phase
causes fibrosis which manifests as
hypertrophic scarring in wounds
(Molan, 2005). If the inflammatory
phase is interrupted by the anti-
inflammatory action of honey, normal
wound contraction occurs resulting in
reduced scarring.
Angiogenesis
Angiogenesis is the formation of new
blood vessels resulting in renewed
supply of new cells and a variety
of growth factors and cytokines —
these regulate the healing process.
›
Practice point
During initial use of honey
dressings, the high osmotic action
may contribute to increased
exudate volume, which could
lead to maceration if the excess
moisture is not managed
appropriately. Manage additional
moisture by adding an absorptive
cover dressing and/or adjusting
the frequency of dressing changes.
This initially increases exudate
in the short term. This should be
clearly explained to the individual
with the wound, who may well
perceive the increase in exudate as
deterioration in their wound.
›
Practice point
Most chronic wounds are ‘stuck’
in a non-healing stage resulting
in defective granulation tissue
formation, and ultimate failure of
the wound to progress through
the proliferation phase of healing
(Boyd et al, 2004). Faced with
chronic wounds on a daily basis,
the ultimate aim of community
nurses is to develop a wound
treatment plan that will ‘kick-
start’ the healing process by
providing an environment which
encourages angiogenesis.
Epidermis
Dermis
Hypodermis
Leptospermum
honey
Wound bed
Exudate
Sloughy tissue
Lymph
Devitalised
tissue
The flow of lymph fluid helps to
rehydrate devitalised tissue
Osmotic action of honey taking lymph from
deeper tissues to bathe the wound bed and
sloughy tissue, creating a moist environment
Figure 1.
Osmotic action of honey.
Honey
dressing