PRESSURE CARE
and family through what can be a
distressing and confusing time. In
the authors’ nursing home there
are open visiting hours and staff
available to answer any questions,
while families are encouraged to
actively participate in decisions
about their relatives’ care. Staff also
This 94-year-old man had undergone a transurethral prostatectomy resection in 2009. Following this surgery he had ongoing
problems with urinary and faecal incontinence and was wheelchair-bound.This led to the development of two category 4
pressure ulcers on the base of his spine and sacrum. He had a long-term self-retaining catheter
in situ,
and, unfortunately,
experienced recurrent hospital admissions from home to hospital for urinary tract infections while multi-resistant strains of
pseudomonas
and meticillin-resistant
Staphylococcus aureus
(MRSA) were confirmed by blood tests and wound swab.
He was admitted into the local hospital in October 2010 with rigors associated with
pseudomonas
contamination and
bacteraemia attributed to his pressure damage and was given a course of intravenous (IV) antibiotics. Finally, At the end of
this period, the patient’s wife was unable to cope with his health needs despite community nurses visiting for day-to-day care,
including the application of Aquacel Ag
®
(ConvaTec) for the bioburden and Allevyn
®
Gentle Border (Smith and Nephew).
Following a meeting with the patient and his wife, he was admitted into the authors’ nursing home for long-term care.
The patient was referred to the tissue viability team on 30 June 2014, due to deterioration in his pressure ulcers. This
was despite the implementation of a robust care pathway. The tissue viability team recommended the use of a gelling
fiber dressing (KytoCel
®
; Aspen Medical), to be applied as a primary dressing. The aim was to reduce the wound’s
bioburden while maintaining a moist wound environment without causing trauma to the pressure ulcers. The patient was
simultaneously prescribed erythromycin and metronidazole for a chest infection. A full care pathway of off-loading and
frequent two-hourly turns was advised, as well as the use of a dynamic mattress with constant skin observations and
hygiene. The patient finally agreed to be nursed in bed for the first time in four years.
Initially, the wound measured 9.5x7cm with significant necrosis and the wound bed was sloughy and very malodourous
with heavy exudate. Dressing retention was difficult due to constant incontinence. However, by 5 August the wound
measured 3x4cm — a reduction of 8cm — while the surrounding tissue had epithelialised with only a small area of
sloughy tissue visible at the base of the spine.
At the time of writing this patient has shown significant improvement and has taken an active role in his pressure-
relieving measures. The wound continues to reduce in size and the authors have every confidence that he will progress to
healing, as demonstrated by a wound swab revealing that MRSA had been irradicated from the wound.
Case report 2
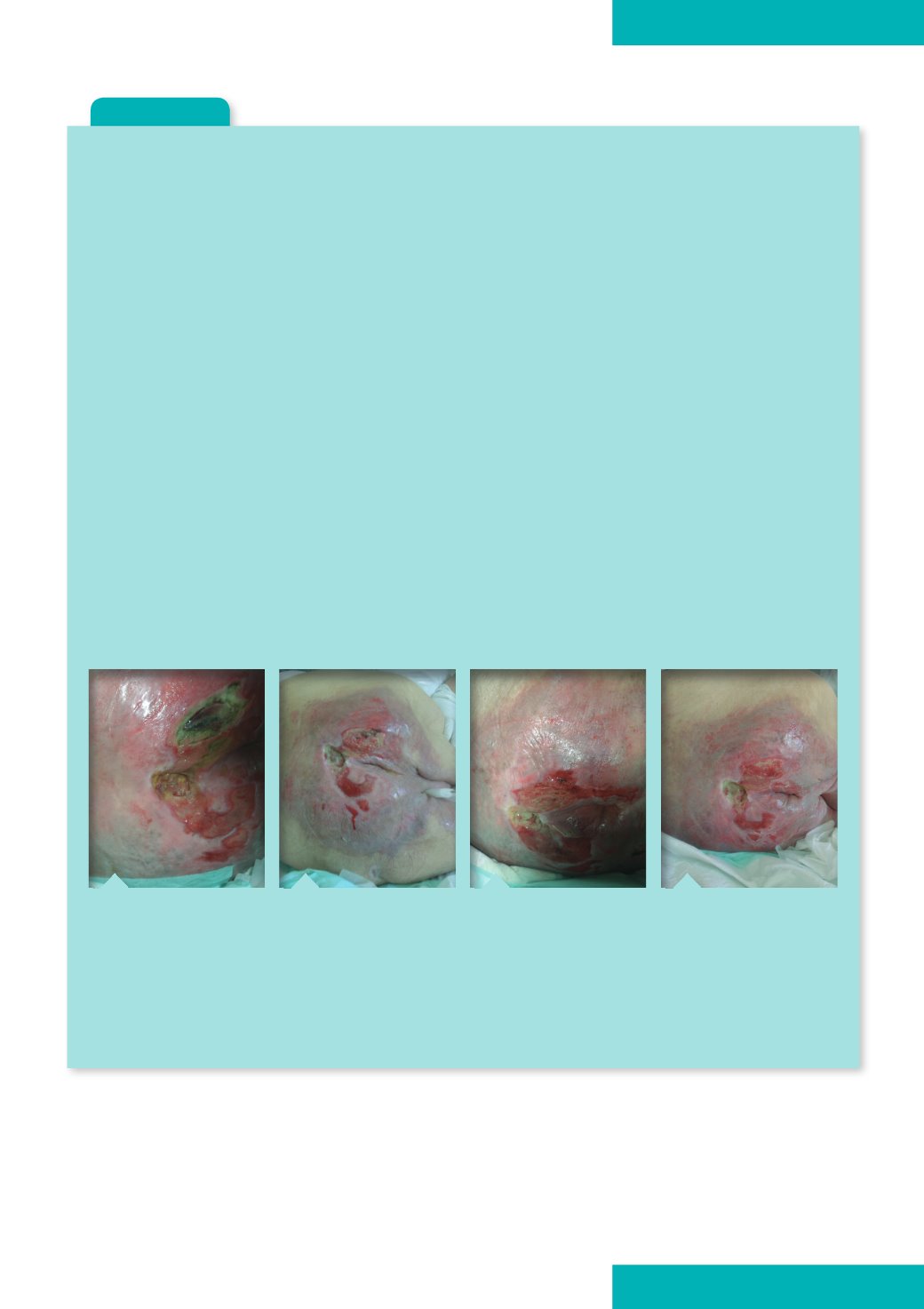
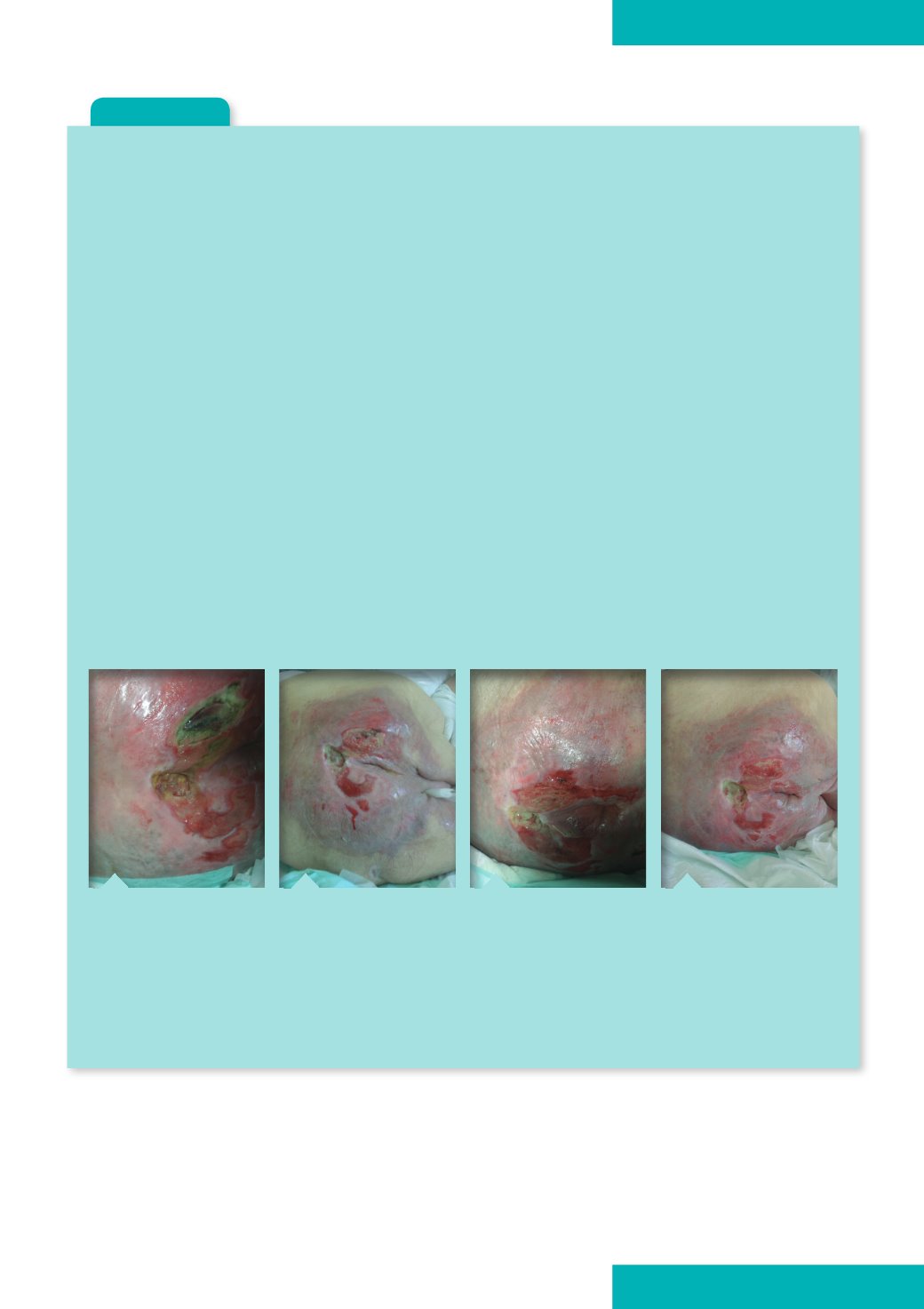
Figure 1.
On 31 May, 2014
the patient had developed
a category 4 pressure ulcer
with moisture damage as
a result of his double
incontinence.
Figure 2.
By 4 June, there
was a visable reduction in
necrotic tissue. Sorbaderm
Barrier Cream (Aspen
Medical) had been
applied to the
surrounding skin.
Figure 3.
On 3 July, any
necrosis had been removed
from the wound bed and
granulation tissue covered
70% of the wound, while
the depth had decreased
by 2cm.
Figure 4.
Later, by 30
September the pressure ulcer
had reduced in size by 8cm.
provide written documentation
regarding pressure ulcers.
As well as looking after the
wound itself, it is important to treat
the patient holistically, bearing in
mind issues such as pain, quality
of life (such as comfort; regular
provision of food and drink;
environment etc), and flexible
visiting times for family. In the
authors’ nursing home, the patients’
next of kin were also present
during consultations with the
specialist team and were given the
opportunity to ask questions.
JCN supplement
2014,Vol 28, No 5
21