36
SKIN CARE TODAY
2015,Vol 1, No 1
FOCUS ON ‘WET’ OR ‘LEAKY’ LEGS
i
approach, such as the one suggested by
Harding et al (2007) with the acronym
HEIDI.This stands for important
aspects of assessing and managing
patients:
i
History — relevant
i
Examination — appropriate
i
Diagnosis — likely or definite
i
Indicators — of progress
or complications.
History
Obtaining a good patient history can
highlight any underlying pathology
that may contribute to oedema and
wet legs. This will include any past or
present history that may reveal any
predisposing factors that influence the
arterial or venous status of the limb,
such as previous episodes of oedema,
ulceration, cellulitis, deep vein
thrombosis (DVT), or varicose veins.
It is also important to find out
if the patient has been previously
treated with compression therapy
and if they were concordant. It should
be established if there is any current
or previous history of immobility
or surgery, which may make ankle
movement difficult or influence
the patient’s ability to use the calf
muscle to aid venous return. The
patient should also be asked how
long the problem has been present
and whether it is bilateral. Cardiac
history, such as stroke or heart disease
and diabetes are relevant, and may
indicate the possible development of
peripheral vascular disease.
Other comorbidities and indicators
that may influence the development
of wet legs may be renal, liver disease,
arthritis. Present prescribed medication
may also contribute to ankle swelling
(Timmons and Bianchi, 2008).
Dietary history is also pertinent,
as malnutrition and low protein may
cause oedema and obesity which may
damage the venous and lymphatic
systems, which, in turn, exacerbates leg
oedema and leg leakage. A referral to
dieticians may be required if an issue
is identified.
The psychological impact of a
wet, leaking leg should always be
considered. Any depression, anxiety
or distress that the problem has
caused should be identified and
discussed, so that interventions
can be put in place to help patients
cope with this often embarrassing
condition (Franks et al, 2006).
Examination
There should be a full examination of
both limbs to observe for skin changes,
oedema, eczema or signs of infection
present. It should also be established
if the symptoms are in one leg or
bilateral.
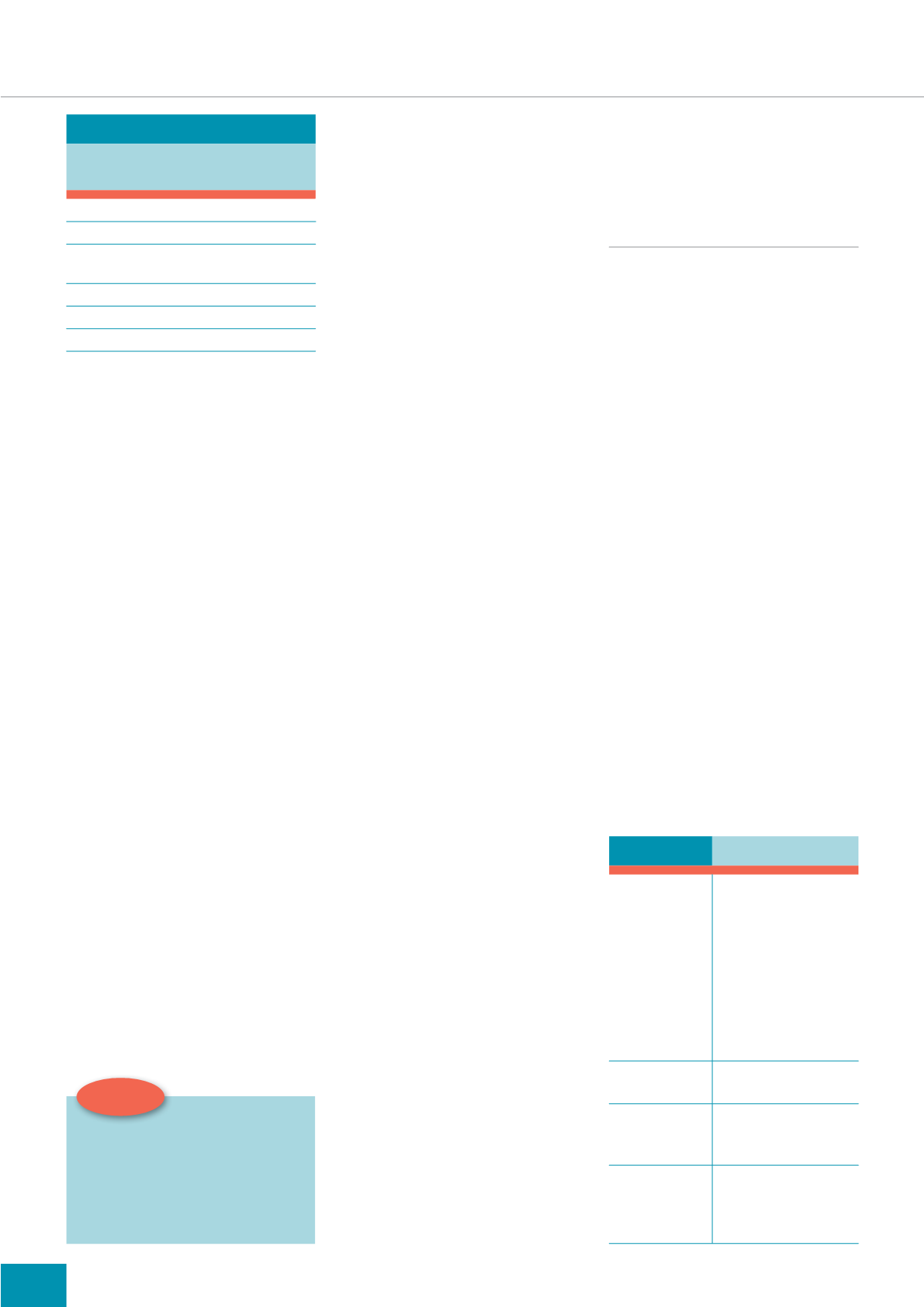
Table 2
illustrates indicators
that should be considered.
Investigations
Full vascular assessment should be
performed to exclude arterial disease
and ensure that the application of
compression is safe.This can be
undertaken by an appropriately trained
clinician with a hand-held Doppler
(Scottish Intercollegiate Guidelines
Network [SIGN], 2010). A normal
ankle brachial pressure index (ABPI)
should measure >0.8. However, this
reading should only be interpreted
in conjunction with other indicators
identified from the holistic assessment.
If the limb is too oedematous, it may be
necessary to perform toe pressures.
Other investigations that may be
appropriate to assist with diagnosis
are C-reactive protein (CRP; infection),
liver function test (LFT; liver failure),
full blood count (FBC; anaemia).
Diagnosis
Once the signs and symptoms, medical
history and investigations are put
together, a diagnosis can be made.This
should guide treatment planning.
MANAGEMENT
In the author’s clinical experience,
management of a wet, oedematous
limb can sometimes be difficult both
for the clinician and patient. Issues
in practice may include manual
handling, as the limb may be heavy
to lift making dressing application
difficult. Two nurses may be needed
to help with redressing legs, or
advice sought from manual-handling
advisors on equipment available to
prevent back injury.
Mobility for the patient often
becomes restricted due to the weight
of the limb. Dressings may become
soggy and heavy causing discomfort
to the patient and resulting in
dressing slippage, which may cause
further trauma to the skin. Leaking
fluid can soil clothing and bed
linen, which may cause distress
and embarrassment to the patient
(Anderson, 2003).
Patient comorbidities, such as
arterial status or cardiac failure, may
influence management options, as high
compression is contraindicated in these
conditions and may have a detrimental
Table 2:
/LPE DVVHVVPHQW
/LPE REVHUYDWLRQ
Observe for skin changes,
such as:
i
Papillomatosis
i
Haemosiderin staining
i
Varicose veins
i
Ankle flare
i
Erythema
i
Eczema
i
Cellulitis
Measure limb
Type of
oedema present
i
Is it bilateral?
i
Is it soft, pitting?
Exudate
i
Colour
i
Amount
i
Consistency
Is ulcer present?
i
Location on the limb
i
Wound measurements
i
Tissue type witin the
wound bed
Table 1:
3RVVLEOH FDXVHV RI FKURQLF
OLPE RHGHPD
Dependency oedema, due to immobility
Heart failure (cardiac oedema)
Venous oedema as a result of venous disease or
severe varicose veins
Obesity
Lymphoedema: both primary and secondary
Oedema associated with cancer
Top tip:
$ KROLVWLF DSSURDFK LV HVVHQWLDO
WR HVWDEOLVK DFFXUDWH GLDJQRVLV
RI WKH XQGHUO\LQJ SUREOHP
DQG IDFLOLDWH GHFLVLRQ PDNLQJ
WKDW HQVXUHV DSSURSULDWH FRVW
HIIHFWLYH SDWLHQW FHQWUHG FDUH